Credentialing Delays Are Costing You More Than You Think
In today’s fast-moving healthcare environment, medical credentialing is the gateway to patient care and revenue generation. Yet, a single overlooked document can stall the entire process—delaying provider onboarding, frustrating staff, and disrupting your cash flow.
Picture this: You’ve just hired Dr. Elsa, a brilliant cardiologist, to enhance your practice’s cardiac care services. But her start date keeps getting pushed back. The issue? An incomplete work history form and a missing state license. While she waits in professional limbo, your patients and profits do too.
Unfortunately, this isn’t an isolated case. Credentialing delays due to missing paperwork are all too common and can have long-term consequences:
The Most Common Credentialing Roadblocks
-
Licenses – State medical license, DEA registration
-
Board Certifications – Proving specialty qualifications
-
Application Forms – Often long, detailed, and error-prone
-
Reference Letters – Required by many hospitals and payers
-
Malpractice Insurance Certificates – Essential for risk coverage
-
Work History Documentation – Must be complete and verifiable
-
Education Credentials – Diplomas from medical school and residency
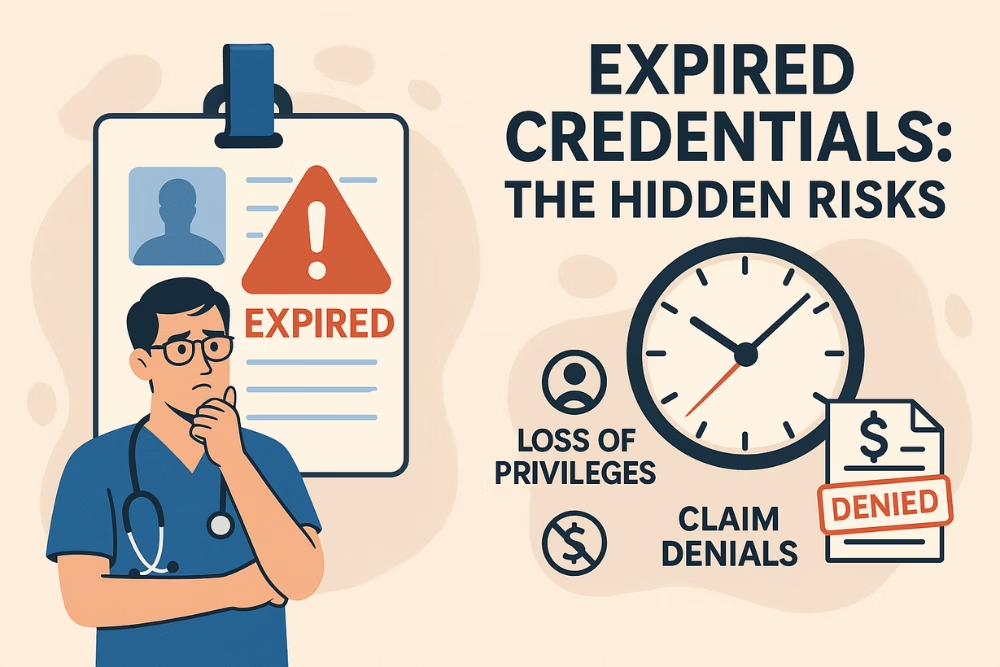
Why Incomplete Documents Derail Everything
-
Credentialing Delays – Chasing paperwork wastes admin time and prolongs onboarding
-
Application Denials – Incomplete submissions often mean starting over
-
Verification Bottlenecks – Delays in primary source verification
-
Provider Frustration – Delays can impact morale and retention
-
Billing & Revenue Stalls – No credentialing = No reimbursement
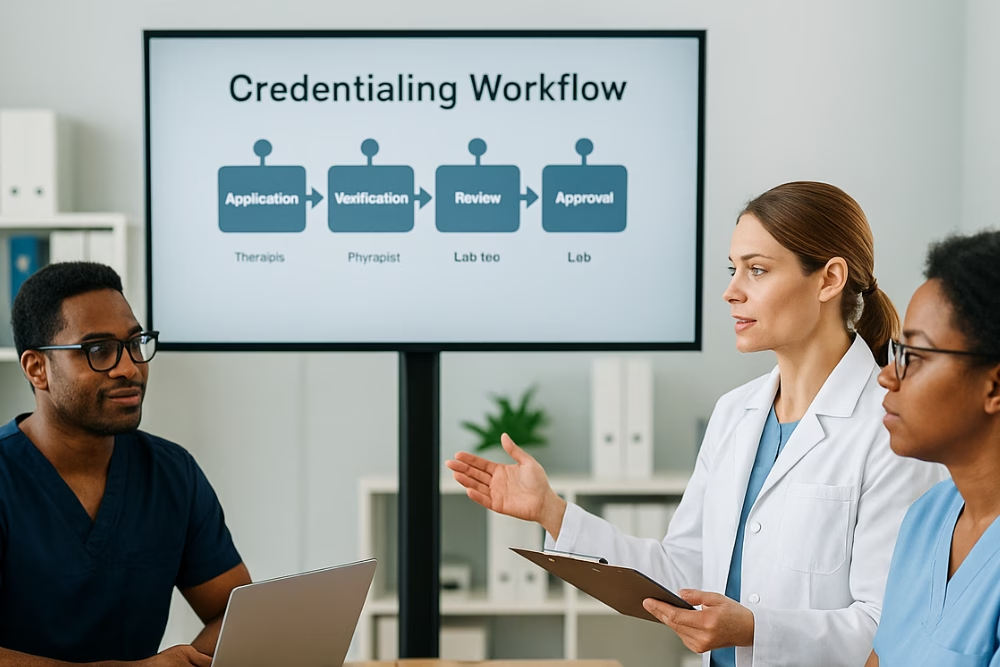
How to Prevent Missing Paperwork Issues
1. Use a Master Checklist
Create a detailed credentialing checklist for every provider. Review and update it regularly based on payer requirements.
2. Set Realistic Timelines
Use project management tools to track credentialing milestones, document submissions, and follow-up timelines.
3. Centralize Document Storage
Adopt a secure digital system (like cloud folders or credentialing software) to manage provider documents.
4. Work With Credentialing Experts
Outsourcing to professionals helps reduce costly mistakes, accelerate processing, and ensure compliance.
5. Maintain Active Communication
Regular follow-ups and open channels between providers and credentialing teams keep things moving smoothly.
Don’t Let Paperwork Derail Your Revenue
Credentialing shouldn’t feel like a guessing game. When you stay proactive, organized, and partner with the right tools, you eliminate the delays that cost your practice time, money, and talent.
➡️ Ready to streamline your credentialing and leave the paperwork headaches behind? Contact the team at eClinicAssist today and discover how our smart solutions keep your credentialing on track and your providers billing faster.