Simplify Provider Credentialing.
Get Credentialed Faster.
Navigating the complexities of provider credentialing doesn’t have to be daunting. At eClinicAssist, we streamline the entire process, reducing enrollment delays and administrative burdens, so you can focus on delivering exceptional patient care.
How eClinicAssist Enhances Your Credentialing Experience
At eClinicAssist, we empower healthcare providers with cutting-edge credentialing solutions. Whether you’re launching a new practice or seeking to enhance the efficiency of an established one, our platform simplifies the complexities of credentialing management.
Transform your workflow, save time, and focus on what matters most—patient care.
Why Choose Our Provider Credentialing Services?
Explore the Benefits of Our Provider Credentialing Services
Our provider credentialing service helps reduce rejections, speed up enrollments, and save your team time.
- Maximize Efficiency: Reduce administrative burdens and focus on patient care.
- Cost-Effective Solutions: Affordable credentialing services designed for every practice size.
- Expert Support: Our dedicated team is here to assist you every step of the way.
- Flexible Integration: Easily integrates with your existing systems for a seamless experience.
Provider Credentialing for Every Practice Size
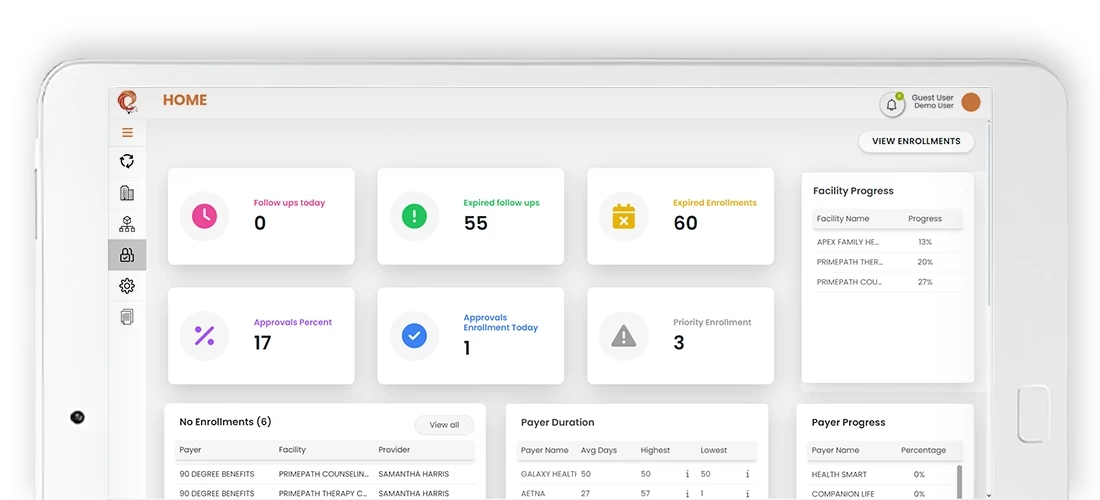
The Provider Credentialing App
Designed for today’s healthcare landscape, our credentialing app is your partner in navigating the complexities of practice management.
From initial application to final approval, experience a seamless journey that enhances accuracy and compliance. With real-time updates, intuitive dashboards, and automated notifications, eClinicAssist ensures your practice stays ahead.
Pricing
Simple pricing. no hidden charges. Choose a plan fit your needs
Package name |
Giveaway |
Essential |
Premium |
|---|---|---|---|
Pricing |
$0 |
$199 per facility$49 per provider |
Get a quote |
| Payor Enrollment & Network Participation | |||
| Credentials Management | |||
| Contract Review & Negotiation | |||
| Recredentialing | |||
| Credentialing Compliance Support | |||
| Revenue Cycle Management | |||
| Credentialing Audit | |||
| Revenue Cycle Management Audit |
At eClinicAssist, we understand the challenges and complexities of navigating the healthcare landscape. Our blog serves as a valuable resource for practice managers, healthcare providers, and industry stakeholders, offering insights and guidance on a variety of critical topics.
Why Your In-Network Claims Still Being Denied? The Credentialing Crisis in Healthcare RCM
The Credentialing Disconnect: Why “In-Network” Doesn’t Guarantee Payment You’ve secured…
Navigating the Malpractice Maze: 7 Essential Risk Management Strategies
Medical malpractice claims are a significant concern for healthcare professionals,…
Why You Must Keep Malpractice Insurance Current for Smooth Credentialing
Why It Matters Now More Than Ever In today’s healthcare…
Contract Review & Negotiation
eClinicAssist offers a comprehensive suite of services designed to eClinicAssist offers a comprehensive suite of services so you can focus on whstreamline the credentialing
Ongoing Compliance Support
eClinicAssist offers a comprehensive suite of services designed to eClinicAssist offers a comprehensive suite of services so you can focus on whstreamline the credentialing
Credentialing
Management
eClinicAssist offers a comprehensive suite of services designed to eClinicAssist offers a comprehensive suite of services so you can focus on whstreamline the credentialing
Provider Credentialing Services That Fit Your Needs
Our provider credentialing services help streamline enrollment and ensure faster payor approvals.