For practice managers, healthcare providers, and owners, provider privileging is a critical process that ensures patient safety and maintains high standards of care. Privileging grants providers the authority to perform specific medical services within a healthcare facility, confirming they have the necessary qualifications, experience, and competence. While closely related to credentialing, privileging goes a step further by defining what a provider can do, not just who they are.
The Three Types of Privileges
Privileges are typically categorized into three main types:
- Admitting Privileges: Allow providers to admit patients to a hospital for inpatient care.
- Courtesy Privileges: Granted to non-affiliated providers who occasionally need to treat patients at the facility.
- Surgical Privileges: Authorize providers to perform specific surgical procedures, often with detailed limitations based on their expertise.
Key Requirements for Privileging
To obtain privileges, providers must demonstrate their competence through:
- Education and Training: Verification of medical degrees, residencies, and specialized training.
- Licensure: A current, unrestricted medical license in the facility’s state.
- Malpractice Insurance: Proof of adequate coverage to protect both the provider and the facility.
- Clinical Experience: Case logs, surgical volumes, and peer attestations.
- Background Checks: Ensuring patient safety and ethical standards.
- Board Certification: Often required for specialized privileges.
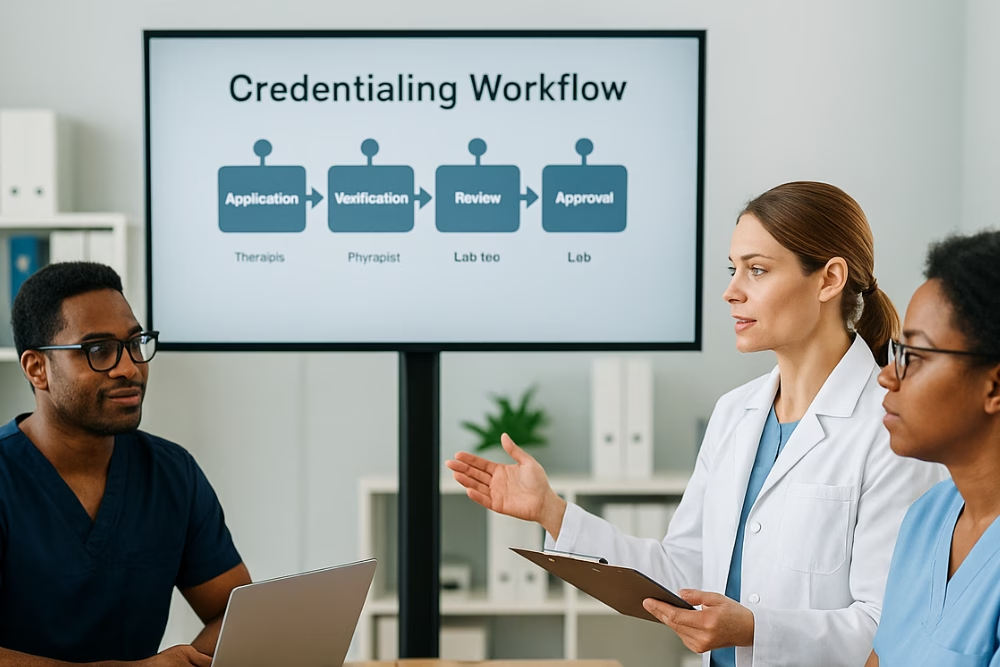
The Privileging Process: Step-by-Step
- Application Submission: Providers submit a detailed application for specific privileges.
- Primary Source Verification: The facility verifies credentials directly with issuing institutions.
- Peer Review: A committee of peers evaluates the provider’s qualifications.
- Credentials Committee Review: Recommendations are made to the medical executive committee.
- Medical Executive Committee Approval: Final approval is granted based on the application and reviews.
- Ongoing Monitoring: Continuous performance reviews ensure quality care and compliance.
Why Privileging Matters
Privileging plays a vital role in:
- Patient Safety: Ensuring only qualified providers perform specific procedures.
- Quality of Care: Maintaining high standards through rigorous competency checks.
- Risk Management: Reducing legal and financial risks for healthcare facilities.
- Resource Allocation: Matching providers with the right skills to the right procedures.
Streamlining the Privileging Journey
Privileging can be complex, but expert credentialing support streamlines it – saving time and resources. From application prep to ongoing monitoring, specialists ensure a smooth process, so providers focus on patient care. Optimize your medical staff’s efficiency and enhance patient outcomes with expert guidance!