Credentialing for Allied Health Professionals — from physical and occupational therapists to dental hygienists and medical assistants — are essential to the fabric of modern healthcare. But behind the scenes, practice managers, healthcare providers, and owners are often caught in a maze of credentialing requirements that slow down onboarding, disrupt patient care, and strain operations.
Credentialing isn’t just another checkbox. It’s the gateway to operational efficiency, provider compliance, and sustained revenue growth. Yet, its complexity stems from a multitude of disciplines — each with its own licensing protocols, payer criteria, and constantly shifting federal and state regulations.
The Challenges: Why Credentialing Feels Like a Maze
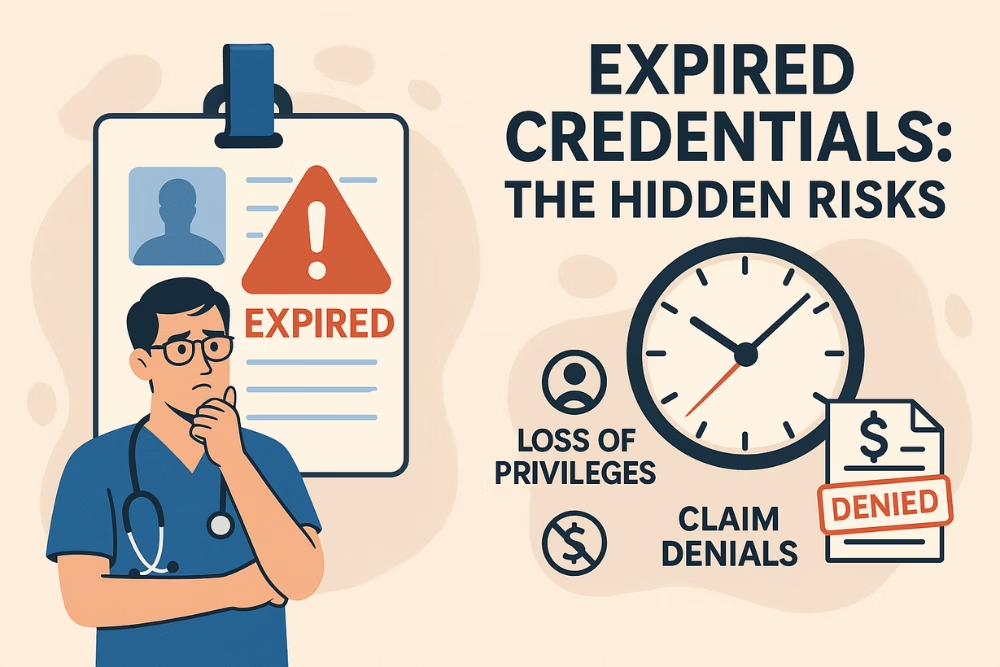
Every profession under the allied health umbrella, whether it’s audiology or respiratory therapy, brings its own credentialing rules. Add to that the inconsistencies between payers and regulatory bodies, and you’ve got a system prone to delays, denials, and bottlenecks.
Common hurdles include:
-
Slow Onboarding: Delayed credentialing extends provider start dates and impacts care delivery.
-
Administrative Overload: Manual data entry and disparate payer forms lead to burnout and errors.
-
Compliance Risks: Misalignment between licensure and scope of practice can cause serious legal and insurance issues.
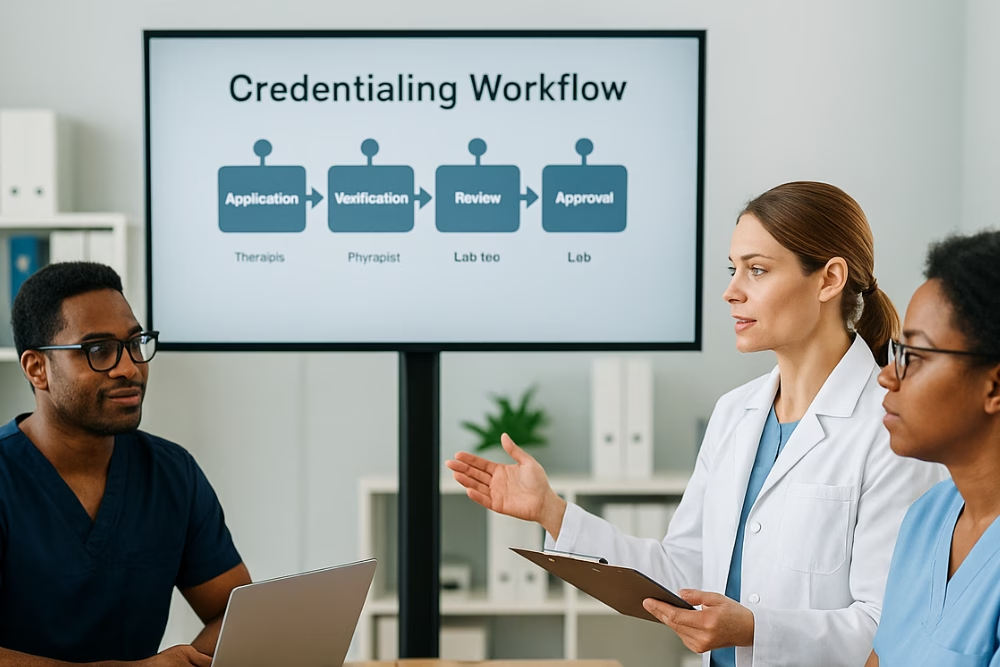
Smart Solutions: How to Simplify and Speed Up Credentialing
You can turn credentialing from a chaotic task into a streamlined process by adopting these modern strategies:
-
Start Early: Begin credentialing as soon as contracts are signed.
-
Ensure Data Accuracy: Implement validation checks to prevent rejections.
-
Train Your Team: Equip staff with regular credentialing education and compliance updates.
-
Go Digital: Use credentialing software for automated data entry, verification, and alerts.
-
Centralize Communication: Keep all parties — providers, staff, and payers — aligned with clear documentation and updates.
-
Use Templates and Checklists: Standardized forms and workflows save time and reduce confusion.
-
Stay Updated: Regularly review payer policies and regulation changes.
Your Solution Partner: eClinicAssist
Navigating allied health credentialing doesn’t have to be overwhelming. At eClinicAssist, we specialize in modernizing the credentialing journey for allied health practices. Our tailored solutions reduce admin burdens, speed up provider onboarding, and improve accuracy across the board.
👉 Let’s simplify your credentialing process today.
Contact eClinicAssist now and discover how our smart tools can help your practice thrive.